Towards a smarter, patient-friendly artificial kidney
What if dialysis could be better?
They are small, silent, and rarely the subject of conversation: our kidneys. Yet every day they filter our entire blood volume an impressive 30 to 50 times. They do so unnoticed, but with a precision that even the most advanced laboratories would envy, until something goes wrong.
Kidney failure affects millions of people worldwide. The gold standard of treatment—kidney transplantation—is not practically or medically possible for every patient. Even those who do qualify for the waiting list face an average wait of two to four years before a suitable donor becomes available.
Most patients are therefore treated with dialysis. The most common form is hemodialysis, an intensive procedure in which blood is filtered outside the body, on average three times a week for four hours at a time. A life-saving therapy, but also highly infrastructure-dependent, costly, and with significant energy and water consumption.
Less visible, but deeply felt by patients, is the physical toll of this treatment. After each session, many suffer from fatigue, dizziness, muscle cramps, or nausea—complaints that severely restrict their daily functioning. Fixed dialysis routines also make it difficult for them to maintain mobility.
Since Dutch physician Willem Kolff developed the first dialysis machine in the 1940s, the basic principles have remained largely unchanged. And so has the impact on patients’ quality of life: time-intensive, physically demanding, and socially limiting.
But what if dialysis could be improved? Not only made more compact, but also more efficient, energy-saving, and patient-friendly?
Today, wearable hemodialysis devices are already in clinical testing—the first step toward miniaturization. Instead of discarding the dialysate after a single round of filtration, it is purified and reused. As a result, only 5 liters of dialysate need to be produced and heated, compared to the usual 120 liters, leading to significant energy savings.
A device that fits in a rolling suitcase also gives patients something many took for granted this summer: the freedom to be away from home for more than a day.
Yet these devices still depend on external blood circuits and complex regeneration systems. Ambitions reach further: better filters, lower costs, and greater autonomy for the patient.
The technological foundations are already there. At imec at Holst Centre, researchers are developing chip-based nanofilters with extremely uniform nanopores. That uniformity is no small detail: it ensures that waste products with small molecular sizes, such as urea and creatinine, are efficiently removed, while larger molecules such as albumin are reliably retained.
Filtration is therefore more sharply defined than with classical dialysis filters, approaching the selectivity of our natural glomeruli. Other organs, such as the lungs, may also benefit from similar chip-based nanofilters tailored for gas exchange.
What also makes such filters remarkable is their scale. They are so thin—just 100 nanometers, or less than one-thousandth the diameter of a hair—that fluid passes through them effortlessly. Thanks to the high pore density, the body’s own blood pressure is sufficient to drive filtration. No external pump is needed, and there is no extra strain on the body.
Nanofilters could thus form the basis for a new generation of dialysis systems: pump-free, with high precision and mechanical stability.
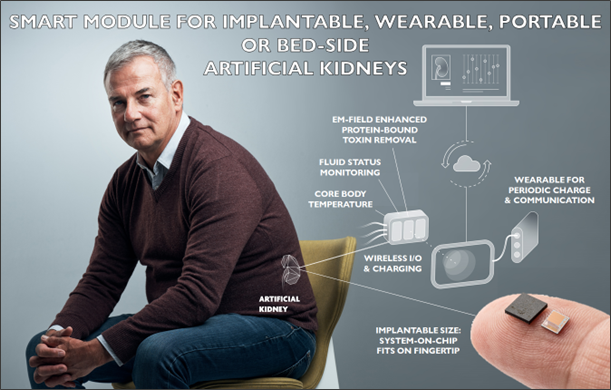
Far-reaching miniaturization of other functions, such as sensors and microelectronics, also makes it possible to build compact, smart systems. In this way, a dialysis system emerges that not only filters, but also continuously monitors vital parameters and transmits them to healthcare providers—real-time data, without patient intervention.
This could open the door to compact, energy-efficient, and patient-friendly solutions that come closer to the natural functioning of the kidney. Think, for example, of night-time home dialysis, an approach that could significantly improve patients’ quality of life compared to the current three hospital sessions per week.
Some researchers are even looking further, towards a fully implantable artificial kidney. This requires a combination of miniaturization, rechargeability, and exceptional biocompatibility—a system that must also function in the body for years. And that is still the greatest challenge.
But moving towards widely usable and smarter solutions demands further development in integrating all the building blocks. This calls for collaboration between the brightest minds in the chip industry, academia, and clinical practice. Thanks to advances in microfluidics, smart sensors, and bioelectronics, the question is no longer if dialysis can become smarter, but how quickly we can make that leap. And above all: how willing policymakers and healthcare systems are to support that transition.
Further information:
The Future of Technology-Based Kidney Replacement Therapies: An Update on Portable, Wearable, and Implantable Artificial Kidneys, Am J Kidney Dis 2025. 85(6):787-796
TechNIERen 4: Chips in dialysis treatment, Fokko Wieringa (YouTube)

